Table of Content
Show a reasonable amount of variation among home health agencies and it should be possible for a home health agency to show performance improvement. We have a pioneering care model with Home Care Connect, our integrated virtual care program that helps patients avoid preventable ER visits and hospitalizations. It enhances our clinical excellence with advanced, easy-to-use remote monitoring technology and 24/7 access to our Virtual Care Center RNs.
This means that following the October 2020 refresh, the data publicly reported will be held constant for all refreshes in 2021, including October 2021. You can find detailed specifications for the claims-based measures in theDownloadssection below. Risk-adjusted outcome measures are identified in theHome Health Outcome Measures Table that is available in theDownloadssection below. The risk adjustment methodology, using a predictive model developed specifically for each measure, compensates for differences in the patient population served by different home health agencies. WebLearn how to identify, develop, launch, and monitor a performance improvement project that will ensure your compliance with the home health CoPs. Risk adjustment is not considered to be necessary for process measures because the processes being measured are appropriate for all patients included in the denominator .
Principal Statistical Programmer
For more information about these process measures, please refer to the Home Health Process Measures Table, which can be located via the link to Home Health Measures Tables in theDownloadssection below. Technical documentation for calculating process measures can be accessed via the link to Technical Documentation of OASIS-Based Measures in theDownloadssection below. The star rating does not include the Willingness to Recommend the HHA item because the results for this item were very similar to those based on the Overall Rating of Care.
The author thanks the staff of Acton Public Health Nursing Service for their support of this project. Identifying "champions" in the agency whose actions supported the project through the challenges that occur during implementation. In addition to assuring early face-to-face contact with the PCPs, educating the patient regarding when to contact the PCP and what information is needed is critical for supporting patient self-management. The author of this article has no significant ties, financial or otherwise, to any company that might have an interest in the publication of this educational activity. Merrily Evdokimoff, RN, MS, was Administrator, Acton Public Health Nursing Service, at the time this article was written. She is currently a PhD candidate at Boston College, Connell School of Nursing, Chestnut Hill, Massachusetts.
You’re signed out
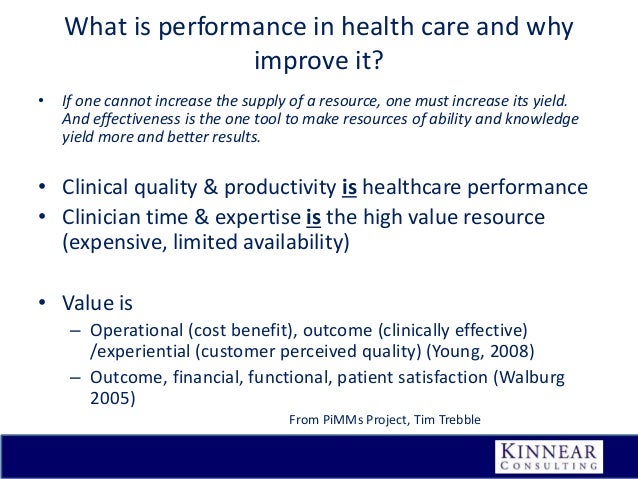
Findings of this study led to the development of four pillars or interventions to resolve these issues identified as creating the most difficulty and turmoil to patients and their care partners following discharge from the hospital (Coleman, 2003; Coleman et al., 2002). While the current draft of the Conditions of Participation for Home Health Agencies Interpretive Guidelines does not provide any guidance regarding what surveyors should look for when it comes to performance improvement projects, there are steps that your agency should follow to ensure compliance. Process measures evaluate the rate of home health agency use of specific evidence-based processes of care. The HH process measures focus on high-risk, high-volume, problem-prone areas for home health care.
Once you have completed the performance improvement project, you will want to report and review the results with your QAPI team. Consider utilizing a storyboard guide for PIPs that can be used to simply and clearly communicate the story of your PIP by providing only the most essential information and including easy to understand graphs and/or charts that clearly demonstrate the impact of your efforts. Process measures are derived from data collected in the OASIS submitted by home health agencies and are calculated using a completed quality episode that begins with admission to a home health agency and ends with discharge, transfer to inpatient facility or sometimes death. For a list of home health outcome measures, please refer to the Home Health Outcome Measures Table, which can be located via the link for Home Health Measures Tables in theDownloadssection below. Technical Specifications for calculating OASIS-based outcome measures, patient-related characteristics measures, and the factors used to risk adjust outcome measures, can be accessed via the link for Technical Documentation of OASIS-Based Measures in theDownloadssection below.
EY-Parthenon (Senior) Manager - Private Equity Value Creation - Transaction and Execution (w/m/d)
CMS base the Patient Survey Star Ratings on the patient experience of care measures. CMS first posted these ratings in January 2016 and CMS post all information about the Patient Survey Star Ratings on theHHCAHPSwebsite. Each HHA gets provider preview reports showing the Quality of Patient Care Star Ratings and rating calculations about 3.5 months before the ratings are posted on Care Compare. On March 26, 2015, CMS sponsored awebinar to review the format of the report and the process for requesting a review of the Quality of Patient Care Star Rating.
Decreasing rehospitalization is a challenge for all sites along the healthcare continuum, but in home healthcare there is often a feeling among staff that the decision to rehospitalize a patient is made by others, without their input. The application of the Four Pillars of Coleman's Care Transition InterventionSM and the special skills of home healthcare clinician can aid in avoiding rehospitalization by teaching the patient appropriate self-management skills. Communication among care providers and patient, family, and other care partners is a necessity in decreasing rehospitalization . The increase in use of hospitalists has further fragmented the communication, as the PCP is often neither aware of the patient's hospital stay nor knowledgeable regarding the new diagnoses and treatments resulting from the hospitalization. Facilitating an appointment with the PCP and/or specialists within 2 weeks of hospital discharge has been shown to decrease hospital readmissions . Assuring the patient has transportation to the appointments is often a critical issue the clinician may be involved in solving.
At MaineHealth, we offer benefits that support an individual's needs for today and flexibility to plan for tomorrow. Our packages include health and dental insurances, paid parental leave, retirement program, generous paid time off, and much more! Our comprehensive array of benefits are competitive, affordable, and include choices that meet specific, but ever changing, needs. Estimated delivery dates - opens in a new window or tab include seller's handling time, origin ZIP Code, destination ZIP Code and time of acceptance and will depend on shipping service selected and receipt of cleared payment. Learn more about situations where an agency may need to develop more than one PIP in a year. The PIP continues after implementation with monitoring, evaluation, and sustainment.
We are deeply invested in the well-being of our communities and care team members. We believe in fostering a work environment of strong commitment, compassionate caring and continuous improvement. Join us, and your abilities will be challenged and enhanced as you take your career to a new level.
Bachelor's degree in systems engineering, healthcare administration, business administration, or other relevant field required. Oversees Agency QA quarterly and annual reporting on QAPI, quality program initiatives. In this chapter we will use a PIP example showing the principles and evidence-based practices are being integrated. Coleman, E., Boult, E., & American Geriatrics Society Health Care Systems Committee. Improving the quality of transitional care for persons with complex care needs. Incorporating the project into current procedures, such as the admission visit, created ease of use and less of an impact on productivity.
Having a Quality Assurance and Performance Improvement program is mandated by the new Home Health Conditions of Participation . While home health agencies should already have their QAPI programs up and running, you have until July 13, 2018 to implement and document at least one performance improvement project to ensure compliance with the CoPs. CMS usually updates the HH QRP claims-based measure results every year. However, due to the COVID-19 Public Health Emergency HHQRP data submission requirements for the Q4 2019, Q1 2020, and Q quarters were exempted. The missing data for Q and Q will impact what is displayed on Care Compare; therefore, public reporting of home health agencies' data will freeze after the October 2020 refresh.
Use analytics from a number of data sources such as Home Health Compare, HHQI reports, CASPER reports, Home Health CAHPS survey results, on-site survey deficiencies, EHR software, and other analytic tools to uncover where performance improvement projects are needed most. You should also consider feedback from patients, families, and staff members as well as “near misses,” incidents, and high-risk situations. The first step in developing a performance improvement project is identifying and prioritizing area for improvement.
Review and apply key points and resources for PIP development and documentation. Tools for the patient may include paper or electronic forms depending on the preference of the patient. In addition, appropriate supports to assure medication compliance such as pillboxes, prepackaged medications, and/or reminder systems may be needed. Of primary importance is assessing the patient's ability and/or willingness to comply with the medication regimen . You’ll also want to evaluate your OASIS accuracy, as documentation errors can inadvertently leave your agency without credit for having initiated care within the proper window. Ensuring accuracy around the entry of OASIS items such as M0104 can make an immediate impact on timely initiation scores.
M&A Business Project Management Manager
This should include initiation of the PIP, planning, implementation, monitoring, and closing. Have changed over time based on the results of ongoing monitoring analyses, technical expert panel input, and stakeholder feedback.

In particular, be sure to equip your patients with the tools they need to understand their condition and treatment plan. By enhancing patient self-efficacy, you can also improve patient activation, adherence, and satisfaction. Also ensure that your clinicians are performing accurate documentation using OASIS in order to demonstrate the right level of patient progress to payers. Complete the following form to learn more about HEALTHCAREfirst’s full service approach to revenue cycle management, CAHPS, and advanced analytics solutions for home health and hospice agencies nationwide. Ensure that the project charter is understood and accepted by all project team members.

No comments:
Post a Comment